Aches and Shakes in the Elderly – By Dr. Gnana Sankaralingam
 Aches and pains in muscles and joints are common occurrences in the elderly. Similarly shakes (tremors) and unsteadiness are phenomenon seen in the process of ageing. While aches and pains could cause disturbance of sleep patterns, tremors and unsteadiness could cause balance problems resulting in falls. Commonly affected are hip and knee joints. Blood supply to muscles in the elderly is compromised due to thickening of the arteries and the resulting ischaemia causing pain due to lactic acid accumulation. Joint pains are due to degenerative changes which results in stiffness due to damage to cartilage which gives low friction surface and reduction of fluid important for lubrication of joint space. Tremors and unsteadiness are caused by problems of neurological and muscular co-ordination. Tremors could involve head, arm or leg, while that of the leg affect manner of walking.
Aches and pains in muscles and joints are common occurrences in the elderly. Similarly shakes (tremors) and unsteadiness are phenomenon seen in the process of ageing. While aches and pains could cause disturbance of sleep patterns, tremors and unsteadiness could cause balance problems resulting in falls. Commonly affected are hip and knee joints. Blood supply to muscles in the elderly is compromised due to thickening of the arteries and the resulting ischaemia causing pain due to lactic acid accumulation. Joint pains are due to degenerative changes which results in stiffness due to damage to cartilage which gives low friction surface and reduction of fluid important for lubrication of joint space. Tremors and unsteadiness are caused by problems of neurological and muscular co-ordination. Tremors could involve head, arm or leg, while that of the leg affect manner of walking.
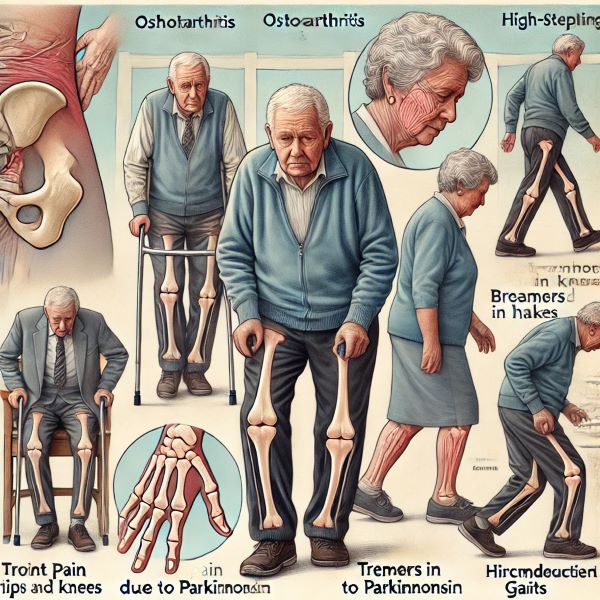
Osteoarthritis is the commonest reason for joint pains. It is characterised by degenerative changes in cartilage and proliferation of new bone and connective tissue, with resultant remodelling of joint contour. By the age of 65, 80% of people have some degree of osteoarthritis visible on X-Ray though only 25% may have symptom. The joints that are most frequently involved are hips, knees, hands and spine. In majority of the patients, the disease is confined to single or few joints. Symptoms onset gradually, with pain intermittent at first, provoked by use of the joint and relieved by rest. As the disease progresses, movements in the affected joint becomes increasingly limited, firstly due to pain and muscular spasm, but later due to changes inside the joint. Treatment is pain relief and rest, with steroid injection into joint cavity. If hip or knee pain result in severe disability, replacement is recommended. Transient episodes of acute neck pain and stiffness occur in the elderly, many precipitated by awkward sleeping posture and most resolve spontaneously within few days. Prolonged neck pain lasting for few months is often a sequel of whiplash (flexion and hyperextension) injury in vehicle collisions, even without fracture or nerve root injury. Cervical spondylosis is common in elderly, which is due to osteoarthritis of spinal joints and associated osteophtye formation. Involvement of nerve roots (radiculopathy) is characterised by radiation of pain along the nerve, numbness, muscle weakness and wasting. Backward movement (Extension of neck) could cause vertigo and drop attacks due to compression of vertibulo-basillar artery in the neck. Most improve with pain killers and soft collar. Those with severe and prolonged pain associated with disc prolapse and radiculopathy, may benefit by traction.
Low back pain can be of mechanical origin or due to other cause. Non specific low back pain of mechanical origin is self limiting resolving spontaneously within few weeks. Chronic low back pains of more than 3 months duration accounts for less than 30% of cases. Episodes of occupationally related low back pain is common in over 40s such as lifting heavy objects, bending or twisting and awkward posture in job. Simple mechanical low back pain is of sudden onset precipitated by bending or lifting, with pain limited to back or thighs and no nerve root distribution. Next common cause is disc prolapse. Each vertebra is separated by a disc from the next one, which acts like a shock absorber. Discs undergo degenerative change due to ageing, and at times protrude beyond their limit. They can prolapse to either right or left or directly backward. Pain radiating down along back of leg beyond knees (sciatica), pain worsened by coughing, sneezing or straining at stool is usually associated with protrusion of disc or compression of nerve root. Simple mechanical low back pains and most of prolapsed discs resolve with rest and pain killers. Resistant cases of disc prolapse may require surgery (laminectomy). Serious low back pain is of insidious onset and progressively worsening, not relieved by rest and pain at night which disturbs sleep. In these, there could be involvement of multiple spinal nerves. There could be secondary deposits from cancers such as prostate, kidney, lungs, breast and thyroid and any elderly presenting with non-mechanical low back pain needs an X-ray of back to exclude secondary deposits. Red flag signs are loss of bowel or bladder control, bilateral sciatica (disc prolapse on both sides), sensory disturbances over genital and anal area due to disc porplapse backward (saddle anaesthesia) or scensory levels on examination. These instances require emergency decompression surgically.
Shakes could occur due to various causes. Cerebellum which is a part of brain controls co-ordination. In cerebellar lesions, shakes occur termed intention tremors, where there is no tremor at rest, but when person tries to move the limb, shaking starts. This is in contrast to resting tremors seen Parkinsonism, where there are pill rolling movements seen at rest, which disappears when person starts moving the limb. Others are flapping tremors seen in liver failure and fine tremors seen in long term usage of asthmatic drugs.
Manner of walking (gait) could be influenced by various factors such as painful joints, balance problem, neuro-muscular and muscular-skeletal issues. Cerebellum a part of brain is concerned with balance and any defect will make the person fall toward the side of the lesion. To prevent falling, they walk with the legs wide apart to make centre of gravity to fall within the base, thus leading to broad-based gait. In lesions of posterior columns of the brain due to diabetes or vitamin B deficiency, person tends to fall onto the opposite side of the lesion. He also loses the ability to know where his feet are. Thus, he walks looking down carefully lifting his feet and placing them firmly on the ground. This is termed high stepping and stamping gait. In Parkinsonism due to lack of dopamine, the muscles become rigid and the person is unable to lift up his thighs. Due to this he drags his feet on the ground termed shuffling gait. If a person suffers a stroke on one side of the body, he is unable to lift thighs on that side and in order to take a step forwards, he rotates his legs outwards (abduction at hip joint) and brings the leg to the front. This is termed circumduction gait. In cerebral palsy where the muscles are rigid, the legs are crossed while walking, called scissor gait. In Painful hip or knee person limps called antalgic gait. In osteomalacia (lack of calcium) and advanced pregnancy as pelvis is unsteady, person wobbles like a duck called waddling gait.
For joint pains, full examination of affected joints such as swelling, tenderness, hotness, deformity and degree of movements deems necessary. For shakes full neurological examination is needed. Investigation for causes of aches and shakes include basic bloods for inflammatory markers, radiography of joints and CT/MRI scan of brain and spine.