Defining Optimal Levels and Doses of Vitamin D for Every Individual – By Dr. Sunil Wimalawansa
Source : grassrootshealth
What should be the minimum vitamin D level among all individuals? What diseases and conditions might benefit from even higher vitamin D levels?
Key Points
- Dr. Sunil Wimalawansa answers several questions, including “Do you recommend an absolute minimum vitamin D level for everyone?,” “In which specific health conditions might an individual choose to have a higher target blood vitamin D level to achieve desired outcomes?,” and “What are the broader benefits of having updated guidelines and barriers to implement?”
- To be clinically effective and to protect all body systems, serum 25(OH)D concentration needs to be “maintained” between 50 to 80 ng/mL range; this would cover approximately 99.9% of all human disorders
- Vitamin D is a threshold micronutrient – its response rates diminish as the blood vitamin D level increases; once reaching the plateau of biological actions, further increased amounts would not provide additional benefit
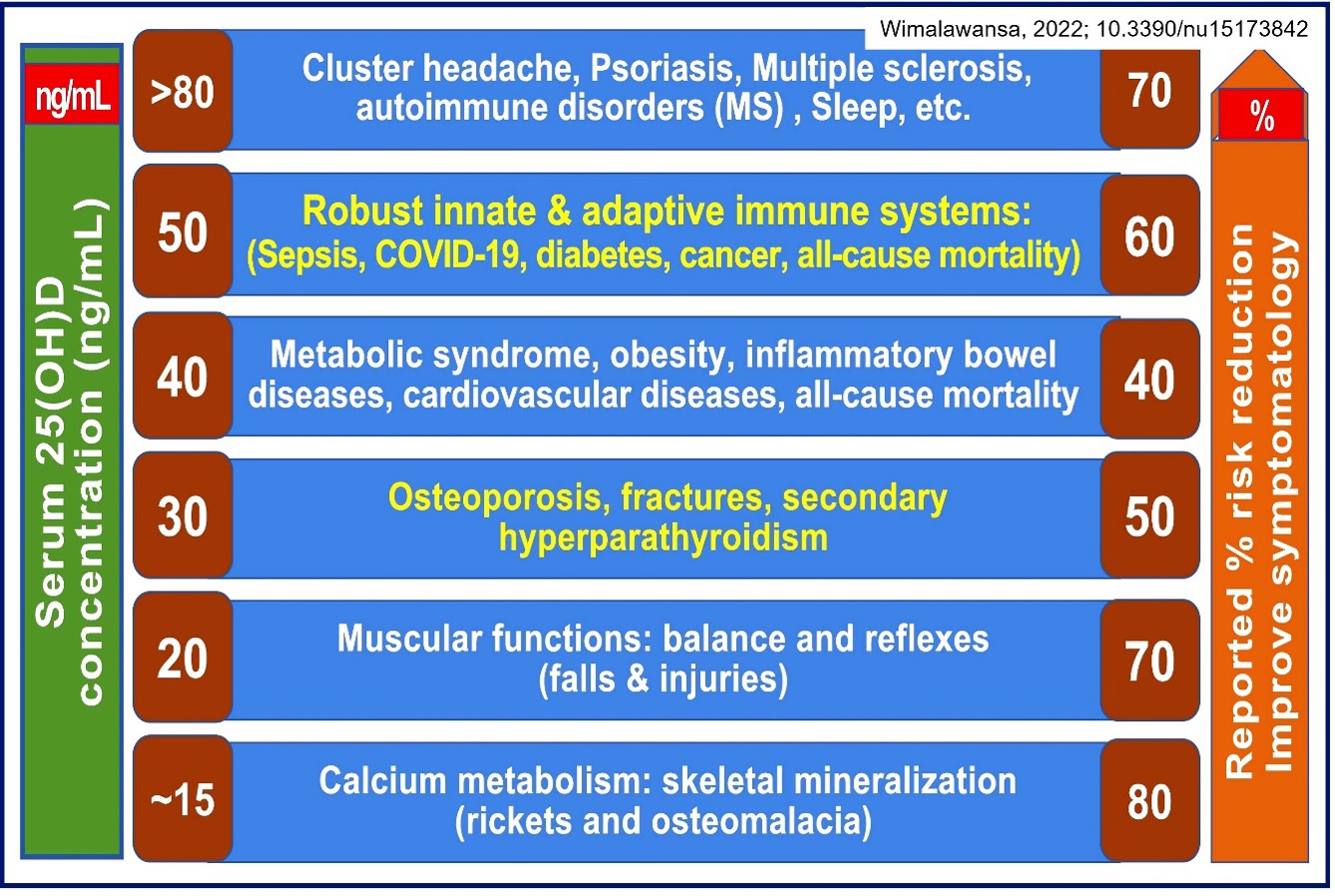
- While musculoskeletal diseases improve with serum 25(OH)D contractions around 20 ng/mL, metabolic disorders need over 40 ng/mL; conditions such as cancer, autoimmune disease, and infections require higher vitamin D intakes to achieve and maintain serum 25(OH)D concentrations above 50 ng/mL
 Dr. Sunil Wimalawansa has been researching vitamin D for over four decades. He is considered one of the world’s leading experts on micronutrients, especially vitamin D. His extensive background includes working with vitamin D: in a laboratory setting, applying his vitamin D knowledge working with patients as a medical doctor, and directing clinical trials involving pharmaceuticals and vitamin D. We introduced Dr. Wimalawansa in Part 1 of this interview series:
Dr. Sunil Wimalawansa has been researching vitamin D for over four decades. He is considered one of the world’s leading experts on micronutrients, especially vitamin D. His extensive background includes working with vitamin D: in a laboratory setting, applying his vitamin D knowledge working with patients as a medical doctor, and directing clinical trials involving pharmaceuticals and vitamin D. We introduced Dr. Wimalawansa in Part 1 of this interview series:Vitamin D: Everything You Need to Know… and More
Today, we will share his answers to questions regarding optimal vitamin D levels and doses and how they vary between individuals.
Questions and Answers with Dr. Wimalawansa
What target vitamin D level do you suggest most individuals should aim to achieve, and what intake amount is most appropriate?
Vitamin D status in a person is determined by measuring serum 25-hydroxy-vitamin D [25(OH)D], which applies to clinical practice and scientific research. 25(OH)D testing should be done in a certified laboratory that takes part in an international quality assurance program. In contrast, 1,25(OH)2D levels do not provide vitamin D status and, thus, should not be requested.
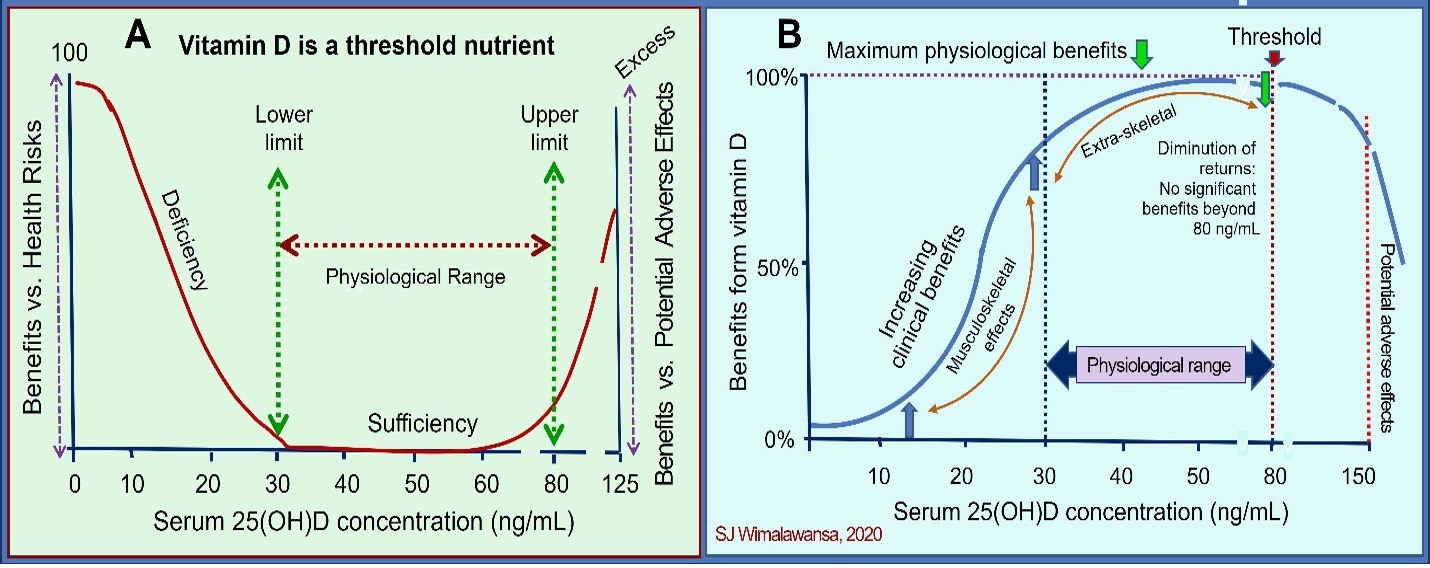
Human biology and tissue (nutritional) physiological “threshold” do not change between healthy vs. sick or young vs. old. However, in evolutionary terms, various body tissues, to function optimally, have adapted different thresholds for micronutrients like vitamin D. What varies between persons is the intake of vitamin D [quantity is expressed as international units (IU) (in some countries use micrograms/day)] needed to achieve and maintain a blood concentration to prevent and overcome disorders.
The mentioned intake requirements to achieve the necessary (target) serum 25(OH)D vary based on the vitamin D status (baseline serum 25(OH)D concentration), medications taken concurrently (like anti-epileptics and anti-retro-viral agents that increase the rate of destruction/catabolism of vitamin D), age, and body mass index (BMI) (weight/fat mass). These principles apply to research and clinical practice; thus, researchers and healthcare workers must know them.
Do you recommend an absolute minimum vitamin D level for everyone?
Over the past three decades, published data confirmed that some body tissues and systems require different serum 25(OH)D concentrations for optimal functions. The minimum serum 25(OH)D must cover all common disorders, not just one condition or tissue like the musculoskeletal system (see DOI: 10.1016/j.jsbmb.2016.09.016). There is no assurance that specific intakes will achieve each person’s needed/target serum 25(OH)D concentration. Therefore, relying on the amount of vitamin D ingested (the dose) to lead to a target serum 25(OH)D is unreliable and unwise. Despite this, medical societies and government-appointed bodies continue (mistaken) blanket recommendations of ‘one dose’ for each age group.
Justifications made based on presumptions or one body system or to favor a particular interest group, whether the minimum serum 25(OH)D concentration is 20 ng/mL (recommended by the Institute of Medicine), 30 ng/mL (The Endocrine Society), or 40 ng/mL (other groups) is irrelevant. Besides, none of these recommended intakes and blood levels can consistently reduce the incidences and severity of critical disorders like cancer, infections, sepsis, autoimmune diseases, or all-cause mortality (DOI: 10.3390/nu15173842).
Consequently, using the minimum serum 25(OH) concentration as level 20, 30, or 40 ng/mL is unhelpful and misleading. Doing so worsens the silo-mentality and confusion among healthcare workers and fails to reduce disease burden and healthcare costs. The following figure demonstrates that various tissues and disease entities respond to different serum 25(OH)D levels.
So, there is no rationale to have different minimal serum vitamin D levels. What would be the most rational minimum serum 25(OH)D level and the range necessary to keep people healthy?
What is essential is to establish the minimum and safe range not for one or another body system or disease but that covers over 99.5% of human disorders without demonstrable adverse effects. This is illustrated in the article—DOI: 10.1016/j.jsbmb.2016.09.016. Based on research published over the past decade, the minimum level should be 50 ng/mL with a target range between 50 to 80 ng/mL. Additional descriptions are illustrated in the following two publications (DOI: 10.3390/nu14142997; DOI: 10.3390/biomedicines11061542). The targeted minimum serum 25(OH)D levels for “communities” is 40 ng/mL, which covers about 80% of disorders.
Dark-skinned people with traditional lifestyles in central Africa have a mean serum 25(OH)D concentration of 47 ng/mL, ranging from 30 to 65 ng/mL, with a healthy upper limit of 80 ng/mL.
To be clinically effective and to protect all body systems, serum 25(OH)D concentration needs to be “maintained” between 50 to 80 ng/mL range. This would cover approximately 99.9% of all human disorders (DOI: 10.3390/nu15173842). Over-exposure to the sun’s UVB rays causes erythema and skin damage and must be avoided. However, excess sun exposure does not overproduce vitamin D or cause hypercalcemia.
You mentioned above that vitamin D is a threshold nutrient. What do you mean by that?
Vitamin D is a threshold micronutrient. Thus, its response rates diminish as the blood vitamin D level increases. Once reaching the plateau of biological actions, further increased amounts would not provide additional benefit (DOI:10.3390/biomedicines11061542: see Figure 4—the dose-response and pharmacodynamic differences between nutrients and pharmaceutical agents). Unlike pharmaceuticals, adverse effects will not appear until serum 25(OH)D concentration reaches very high levels.
This principle is crucial when designing RCTs—recruiting only those vitamin D deficient into clinical studies. This criterion was noted in the Nutrient Study Guidelines by Dr. Robert Heaney, outlined here.
Why do some conditions require a higher intake of vitamin D and serum 25(OH)D concentrations to improve?
Even today, the government and its agencies recommend doses of vitamin D between 400 and 800 IU. This was 30 years ago aimed to maintain serum 25(OH)D concentration around 20 ng/mL to prevent rickets and osteomalacia (musculoskeletal needs), based on research done in the 1980s. Those studies confirmed that these minute amounts are sufficient to prevent the occurrence of rickets in children and osteomalacia in adults, but nothing else. Ironically, some scientists and physicians continue to hang on to this obsolete data that does not help the public.
In contrast, nature has allowed a person with fair skin, with a third of the upper body exposed to direct sunlight between 10.30 AM and 1.30 PM (with the eyes and face protected from UV/sunlight), to generate up to 10,000 IU (~250 micrograms) vitamin D/day from ultra-violet B (UVB) rays, affirming generating or ingesting 10,000 IU/daily is safe (DOI: 10.1007/978-0-387-77574-6_1:1-15). Thus, it is unsurprising that humans need about ten-fold higher vitamin D intakes than the government-recommended doses and higher serum 25(OH)D concentrations.
While musculoskeletal diseases improve with serum 25(OH)D contractions around 20 ng/mL, metabolic disorders need over 40 ng/mL. Conditions such as cancer, autoimmune disease, and infections require higher vitamin D intakes to achieve and maintain serum 25(OH)D concentrations above 50 ng/mL—higher than the current 30 ng/mL recommended by most scientific societies. The latter is because these recommendations are outdated.
Although in small numbers, other conditions respond to even higher serum 25(OH)D concentration, like above 80 ng/mL. Rare genetic disorders like calcitriol/vitamin D receptor variants (pleomorphism and mutations) cause lesser affinity to calcitriol, requiring much higher doses and maintaining a higher serum 25(OHD concentration (DOI: 10.1016/j.rdc.2012.03.009). Other specific conditions require higher serum 25(OH)D concentrations for better clinical responses. To overcome these disorders, such patients are treated with much higher doses of D3 and maintain higher serum 25(OH)D concentrations, usually above 80 ng/mL. Such clinical practice protocols include the Coimbra protocol (DOI: 10.3390/nu14081575) and others (DOI: 10.1016/j.jsbmb.2018.12.010). As discussed, these procedures must be managed under close medical supervision. These few disorders need higher (therapeutic) pharmacological doses of vitamin D to overcome defects and produce the desired clinical outcomes.
In which specific health conditions might an individual choose to have a higher target blood vitamin D level to achieve desired outcomes?
As discussed, maintaining the minimum (50 ng/mL;125 nmol/L) and the optimum range of serum 25(OH)D (50 to 80 ng/mL) concentration will cover 99.9% of the disorders affecting humans (DOI: 10.3390/nu15173842). As we witnessed during the COVID-19 pandemic (and so will be in future endemics and pandemics), maintaining a higher than the currently recommended serum 25(OH)D concentrations is essential to minimize infection-related symptomatic diseases, hospitalizations, and deaths, and sepsis-related deaths. Data strongly suggests that maintaining serum 25(OH)D concentrations “above 50 ng/mL” is the optimum to provide the broadest protection in humans with no adverse effects.
In contrast, if one considers 80 ng/mL as the minimum level (associated with a large scatter of distribution) while covering 99.99% of health conditions, it will cause unacceptably higher adverse effects, thus unjustified. Only less than 0.01% of the (global) population requires a higher minimum serum 25(OH)D concentrations to overcome specific conditions and disorders. Examples requiring higher serum 25(OH)D concentrations (above 80 ng/mL) include vitamin D-resistant genetic disorders/syndromes, intractable migraine/cluster headaches, drug-resistant psoriasis, asthma, certain autoimmune diseases, and to prevent tissue and organ graft rejection.
Note: Persons who wish to or are undergoing high doses of vitamin D to overcome the mentioned disorders must be managed under strict medical supervision on an individual basis. They need to find a specialist (preferably locally) with experience, willing to work using high (pharmacological) doses of vitamin D to maximize benefits and minimize adverse effects. Preferably managed in a specialized center with facilities to rapidly measure blood and urinary variables while patients are in the clinic. Nevertheless, according to common sense and medical ethics, healthcare workers must strike a safe amount for a given condition to obtain maximum benefits while avoiding adverse effects (Hippocratic Oath).
What conditions have you found are most responsive to vitamin D?
Vitamin D deficiency causes various signs and symptoms; because of its chronic and insidious nature, many may not have or present with classical signs or symptoms; they could be asymptomatic until levels decrease below 10 ng/mL. Rickets in children and osteomalacia in adults are the two most responsive clinical conditions that respond to vitamin D. I had many older persons who were wheel-chair bound, dependent on their families for day-to-day activities—high dose vitamin D allowed them to get back to normality within a short period. The lower the serum 25(OH)D concentration, the higher (and rapid) the responses are.
Clinical suspicion is essential to make a clinical diagnosis. Be proactive in testing serum 25(OH)D concentrations when facilities are available and covered by insurance. If clinically suspected of having vitamin D deficiency, one can send a blood sample for laboratory testing, but no need to wait for results to materialize. They can be treated with a one-time, high dose of vitamin D3 (between 100,000 and 300,000 IU), followed by a daily or weekly maintenance dose—as a therapeutic trial is appropriate. Unsurprisingly, correcting such deficiencies improves or eliminates signs or symptoms of musculoskeletal disorders. In all other conditions, vitamin D should be an adjunct therapy with best practices, such as using antibiotics for infections.
Why does the same dose in people have different results?
Not everyone has the same sensitivity to nutrients or medications: i.e., the same dose has different responses among individuals, depending on the baseline serum 25(OH)D concentration (starting level), genetic makeup, body mass index (fat and muscle mass), etc. It also varies with the genetic constraints, dose and intake frequency, and underlying metabolic situations.
In addition, individual responses vary for other reasons, such as epigenetic modifications, environmental issues, internal milieu, coexisting and co-morbid conditions, and medications taken concomitantly, like anti-epileptics or antiretroviral agents. Another variability for different sensitivity and responses is due to vitamin D receptor pleomorphism and genetic variants of cytochrome P450 (CYP) genes that express various vitamin D-related enzymes (e.g., vitamin D-resistant rickets; genetic abnormalities of CYP enzymes).
Why is there an increased need to take higher amounts of vitamin D?
With globalization, over the past five decades, there have been significant socio-economic changes across the globe. The gap between the rich and the poor widens while the percentage of the economically poor sector escalates. Meanwhile, poverty and air pollution have tripled. Sicknesses including chronic ill-health like type 2 diabetes, obesity, metabolic syndrome, cancer, and childhood disorders, and the resultant untimely deaths, including from pharmaceuticals, are explored, adding to the cost of healthcare.
Meanwhile, globalization-driven, attractive, misleading advertising has destroyed healthy habits, balanced diets, and lifestyles. It increased the processed and fast-food industry with parallel deterioration of the quality of processed and fast foods, associated with eating fewer fresh vegetables (less roughage and anti-oxidants). This worsened nutrient imbalance with lesser intakes of micronutrients and have led to an increased need for higher vitamin D intake and the serum 25(OH)D concentrations necessary to tackle ongoing health problems, including obesity, diabetes, cancer, and infections.
How should we tackle these broader issues related to healthcare, sickness, and costs?
We need fundamental changes in personal habits—revert to healthier lifestyles and eating habits— eating family meals more at home, re-introducing home gardening, etc. Public education programs should also curtail the current trend of ‘pharma-driven’ reliance on medications rather than a healthy balanced diet and daily home-based physical activities to keep healthy. Doing so will dramatically improve the nation’s health, minimize absenteeism, and reduce healthcare costs. However, implementing these straightforward measures is thwarted because of conflicts of interest and the lack of vision by politicians and administrators.
We estimate that having a balanced diet with micro-nutrient sufficiency, with a minimum of 30 minutes of day-to-day physical activity at home or in the community (not gym-based), within a few years will reduce the acute and chronic disease burden (morbidity), hospitalization, and premature deaths (mortality) by 50%. Adhering to such will reduce the need for doctors’ visits and the use of pharmaceuticals by 60%. Vitamin D sufficiency plays a crucial role here.
What are the broader benefits of having updated guidelines and barriers to implement?
Vitamin D is a generic micronutrient available worldwide without prescriptions. D3 is the only vitamin D to take as a supplement, not expensive vitamin D metabolites or analogs. In the West, it costs less than $6 per year supply, or as an adjunct therapy, it costs about $2 to prevent or treat an acute disease like SARS-CoV-2 infection. Maintaining circulatory levels of 25(OH)D above 50 ng/mL, with daily or once-a-week vitamin D supplements or safe sun exposure, would reduce the prevalence and the severity of most chronic diseases and some acute illnesses like infections.
On average, eliminating vitamin D deficiency costs less than 0.1% of the cost of investigations and treatment of worsening comorbidities and complications associated with hypovitaminosis D, including COVID-19 (DOI: 10.3390/biology8020030). For example, the average cost of managing vitamin D deficiency-associated diseases (e.g., diabetes, obesity, multiple sclerosis, etc.) and related complications is between $5,000 to $18,000/year [Reducing Risks from COVID-19: Cost-Effective Ways of Strengthening Individual’s and the Population Immunity with Vitamin D (endocrinoljournal.com)]. The average cost-benefits of using vitamin D as a prophylactic agent exceed 1: 10,000.
This is good news for ordinary people who live a healthier life longer with fewer illnesses and expenses, but bad news for big pharma. Consequently, big pharma, some conflicted individuals and philanthropies, medical societies, leading health organizations, and government-appointed committees continuously downplay the importance of vitamin D. This is unsurprising, as they rely on pharma money and perks—consequently refusing to update the grossly outdated vitamin D guidelines, which harm millions.
* The above is a scientific discussion and should not be considered medical advice. Regarding clinical or personal issues, Prof. Wimalawansa advises readers to consult her/his physician.